What is chronic pain?
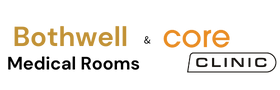
Pain starts in receptor nerve cells found beneath the skin and in organs throughout the body. When you are sick, injured, or have other type of problem, these receptor cells send messages along nerve pathways to the spinal cord, which then carries the message to the brain. Pain medicine reduces or blocks these messages before they reach the brain.
Pain can be anything from a slightly bothersome, such as a mild headache, to something excruciating and emergent, such as the chest pain that accompanies a heart attack, or pain of kidney stones. Pain can be acute, meaning new, subacute, lasting for a few weeks or months, and chronic, when it lasts for more than 3 months.
Chronic pain is one of the costliest health problems in the world. Increased medical expenses, lost income, lost productivity, compensation payments, and legal charges are some of the economic consequences of chronic pain.
Consider the following:
- Low back pain is one of the most significant health problems. Back pain is a common cause of activity limitation in adults.
- Cancer pain affects most people with advanced cancer.
- Arthritis pain affects more than 8 million each year in the UK.
- Headaches affect millions of adults. Some of the most common types of chronic headaches are migraines, cluster headaches, and tension headaches.
- Other pain disorders such as the neuralgias and neuropathies that affect nerves throughout the body, pain due to damage to the central nervous system (the brain and spinal cord), as well as pain where no physical cause can be found--psychogenic pain--increase the total number of reported cases.
What are the different types of pain?
Two types of pain include the following:
- Acute pain. This pain may come from inflammation, tissue damage, injury, illness, or recent surgery. It usually lasts less than a week or two. The pain usually ends after the underlying cause is treated or has been resolved.
- Chronic pain. Pain that persists for months or even years.
What is chronic pain?
Chronic pain is long standing pain that persists beyond the usual recovery period or occurs along with a chronic health condition, such as arthritis. Chronic pain may be "on" and "off" or continuous. It may affect people to the point that they can't work, eat properly, take part in physical activity, or enjoy life.
Chronic pain is a major medical condition that can and should be treated.
What causes chronic pain?
There are many causes of chronic pain. It may have started from an illness or injury, from which you may have long since recovered from, but pain remained. Or there may be an ongoing cause of pain, such as arthritis or cancer. Many people suffer chronic pain in the absence of any past injury or evidence of illness.
What is the "terrible triad?"
When pain becomes such a problem that it interferes with your life's work and normal activities, you may become the victim of a vicious circle. Pain may cause you to become preoccupied with the pain, depressed, and irritable. Depression and irritability often leads to insomnia and weariness, leading to more irritability, depression, and pain. This state is called the "terrible triad" of suffering, sleeplessness, and sadness. The urge to stop the pain can make some people drug-dependent, and may drive others to have repeated surgeries, or resort to questionable treatments. The situation can often be as hard on the family as it is on the one suffering with the pain.
How is chronic pain treated?
Chronic pain affects all parts of your life. The most effective treatment includes symptom relief and support. A multidisciplinary approach to pain management is often required to provide the needed interventions to help manage the pain. Pain management programs are usually done on an outpatient basis. Many skilled professionals are part of the pain management rehabilitation team, including:
- Neurologists and neurosurgeons
- Orthopaedists and orthopaedic surgeons
- Anaesthesiologists
- Oncologists
- Physiatrists
- Nurses
- Physical therapists
- Occupational therapists
- Psychologists/psychiatrists
- Social workers
- Case managers
- Vocational counsellors
Special pain programs are located in many hospitals, rehab facilities, and pain clinics.
Our pain management rehab program
A pain management rehab program is designed to meet your needs. The program will depend on the specific type of pain, disease, or condition. Active involvement by you and your family is vital to the success of the program.
The goal of pain management programs is to help you return to the highest level of function and independence possible, while improving the overall quality of life--physically, emotionally and socially. Pain management techniques help reduce your suffering.
To help reach these goals, pain management programs may include:
- Medical management of chronic pain, including medicine management:
- Over-the-counter (OTC) medicines may include nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin etc.
- Prescription pain medicines, including opioids, may be needed to provide stronger pain relief than aspirin. However, these drugs are reserved for more severe types of pain, as they have some potential for abuse and may have unpleasant and potentially very dangerous side effects.
- Prescription antidepressants can help some people. These medicines increase the supply of the naturally produced neurotransmitters, serotonin and norepinephrine. Serotonin is an important part of a pain-controlling pathway in the brain.
- Heat and cold treatments to reduce the stiffness and pain, especially with joint problems such as arthritis.
- Physical and occupational therapy such as massage and whirlpool treatments
- Exercise to reduce spasticity, joint contractures, joint inflammation, spinal alignment problems, or muscle weakening and shrinking to prevent further problems
- Local electrical stimulation involving application(s) of brief pulses of electricity to nerve endings under the skin to provide pain relief
- Injection therapies, such as epidural steroid injection
- Emotional and psychological support for pain, which may include the following:
- Psychotherapy and group therapy
- Stress management
- Relaxation training
- Meditation
- Hypnosis
- Biofeedback
- Behavior changes
The philosophy common to all of these varied psychological approaches is the belief that you can do something on your own to control pain. This includes changing your attitudes, the perception of being a victim, feelings, or behaviors associated with pain, or understanding how unconscious forces and past events have contributed to pain.
- Patient and family education and counseling
- Alternative medicine and therapy treatments, as appropriate
In addition, treatment may include:
- Surgery. Surgery may be considered for chronic pain. Surgery can bring release from pain, but may also destroy other sensations as well, or become the source of new pain. Relief is not necessarily permanent, and pain may return. There is a variety of operations to relieve pain. Consult your doctor for more information.
Acupuncture. Acupuncture is a 2000-year-old Chinese technique of inserting fine needles under the skin at selected points in the body and has shown some promise in the treatment of chronic pain. Needles are manipulated by the practitioner to produce pain relief. What are the different types of pain?
Two types of pain include the following:
- Acute pain. This pain may come from inflammation, tissue damage, injury, illness, or recent surgery. It usually lasts less than a week or two. The pain usually ends after the underlying cause is treated or has been resolved.
- Chronic pain. Pain that persists for months or even years.
What is chronic pain?
Chronic pain is long standing pain that persists beyond the usual recovery period or occurs along with a chronic health condition, such as arthritis. Chronic pain may be "on" and "off" or continuous. It may affect people to the point that they can't work, eat properly, take part in physical activity, or enjoy life.
Chronic pain is a major medical condition that can and should be treated.
What causes chronic pain?
There are many causes of chronic pain. It may have started from an illness or injury, from which you may have long since recovered from, but pain remained. Or there may be an ongoing cause of pain, such as arthritis or cancer. Many people suffer chronic pain in the absence of any past injury or evidence of illness.
What is the "terrible triad?"
When pain becomes such a problem that it interferes with your life's work and normal activities, you may become the victim of a vicious circle. Pain may cause you to become preoccupied with the pain, depressed, and irritable. Depression and irritability often leads to insomnia and weariness, leading to more irritability, depression, and pain. This state is called the "terrible triad" of suffering, sleeplessness, and sadness. The urge to stop the pain can make some people drug-dependent, and may drive others to have repeated surgeries, or resort to questionable treatments. The situation can often be as hard on the family as it is on the one suffering with the pain.
How is chronic pain treated?
Chronic pain affects all parts of your life. The most effective treatment includes symptom relief and support. A multidisciplinary approach to pain management is often required to provide the needed interventions to help manage the pain. Pain management programs are usually done on an outpatient basis. Many skilled professionals are part of the pain management rehabilitation team, including:
- Neurologists and neurosurgeons
- Orthopedists and orthopedic surgeons
- Anesthesiologists
- Oncologists
- Physiatrists
- Nurses
- Physical therapists
- Occupational therapists
- Psychologists/psychiatrists
- Social workers
- Case managers
- Vocational counselors
Special pain programs are located in many hospitals, rehab facilities, and pain clinics.
The pain management rehab program
A pain management rehab program is designed to meet your needs. The program will depend on the specific type of pain, disease, or condition. Active involvement by you and your family is vital to the success of the program.
The goal of pain management programs is to help you return to the highest level of function and independence possible, while improving the overall quality of life--physically, emotionally and socially. Pain management techniques help reduce your suffering.
To help reach these goals, pain management programs may include:
- Medical management of chronic pain, including medicine management:
- Over-the-counter (OTC) medicines may include nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, or acetaminophen.
- Prescription pain medicines, including opioids, may be needed to provide stronger pain relief than aspirin. However, these drugs are reserved for more severe types of pain, as they have some potential for abuse and may have unpleasant and potentially very dangerous side effects.
- Prescription antidepressants can help some people. These medicines increase the supply of the naturally produced neurotransmitters, serotonin and norepinephrine. Serotonin is an important part of a pain-controlling pathway in the brain.
- Heat and cold treatments to reduce the stiffness and pain, especially with joint problems such as arthritis
- Physical and occupational therapy such as massage and whirlpool treatments
- Exercise to reduce spasticity, joint contractures, joint inflammation, spinal alignment problems, or muscle weakening and shrinking to prevent further problems
- Local electrical stimulationinvolving application(s) of brief pulses of electricity to nerve endings under the skin to provide pain relief
- Injection therapies, such as epidural steroid injection
- Emotional and psychological support for pain, which may include the following:
- Psychotherapy and group therapy
- Stress management
- Relaxation training
- Meditation
- Hypnosis
- Biofeedback
- Behavior changes
The philosophy common to all of these varied psychological approaches is the belief that you can do something on your own to control pain. This includes changing your attitudes, the perception of being a victim, feelings, or behaviors associated with pain, or understanding how unconscious forces and past events have contributed to pain.
- Patient and family education and counseling
- Alternative medicine and therapy treatments, as appropriate
In addition, treatment may include:
- Surgery may be considered for chronic pain. Surgery can bring release from pain, but may also destroy other sensations as well, or become the source of new pain. Relief is not necessarily permanent, and pain may return. There is a variety of operations to relieve pain. Consult your doctor or more information.
- Acupuncture is a 2000-year-old Chinese technique of inserting fine needles under the skin at selected points in the body, and has shown some promise in the treatment of chronic pain. Needles are manipulated by the practitioner to produce pain relief.
What is Nerve Pain?
What causes neuropathic pain?
There are many reasons that patients may develop neuropathic pain. However, on a cellular level, one explanation is that an increased release of certain neurotransmitters which signal pain, combined with an impaired ability of the nerves to regulate these signals leads to the sensation of pain originating from the affected region. Additionally, in the spinal cord, the area which interprets painful signals is rearranged, with corresponding changes in neurotransmitters and loss of normally functioning cell bodies; these alterations result in the perception of pain even in the absence of external stimulation. In the brain, the ability to block pain can be lost following an injury such as stroke or trauma. Over time, further cellular damage occurs, and the sense of pain persists.
Neuropathic pain is associated with diabetes, chronic alcohol intake, certain cancers, vitamin B deficiency, infections, other nerve-related diseases, toxins, and certain drugs.
What are the signs and symptoms of neuropathic pain?
Unlike other neurological conditions, identification of neuropathic pain is hard. Few, if any, objective signs are present. Examiners have to decipher and interpret a collection of words that patients use to describe their pain. Patients may describe their symptoms as sharp, dull, hot, cold, sensitive, itchy, deep, stinging, burning, or some other descriptor. Additionally, some patients may feel pain with a light touch or pressure.
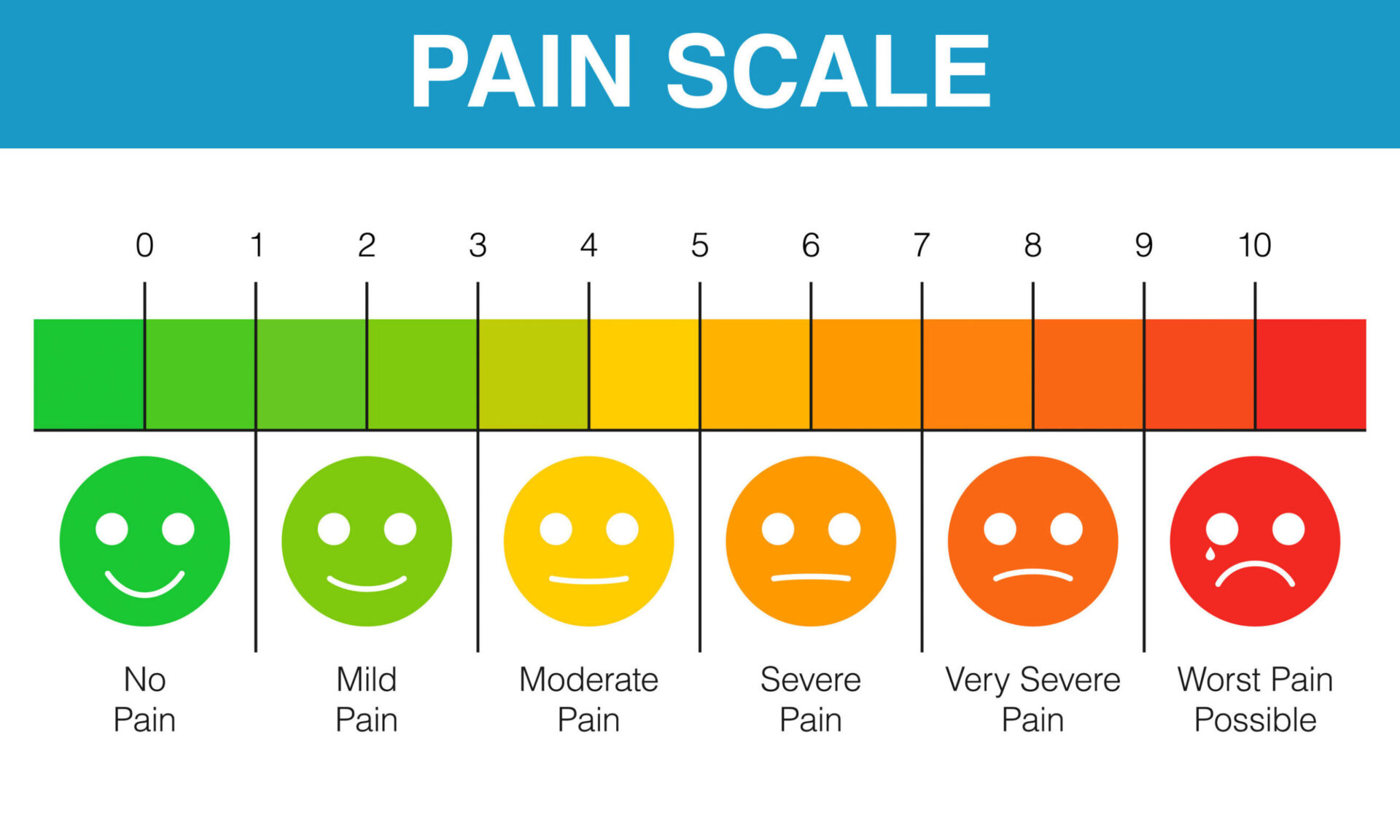
In an effort to help identify how much pain patients may be experiencing, different scales are often used. Patients are asked to rate their pain based on a visual scale or numeric graph. Many examples of pain scales exist. Often, pictures of faces depicting various degrees of pain can be helpful when patients have a difficult time describing the amount of pain they are experiencing.
How do doctors diagnose neuropathic pain?
The diagnosis of pain is based upon further assessment of a patient's history. If underlying nerve damage is suspected, then evaluation of the nerves with testing may be warranted. The most common way to evaluate whether a nerve is injured is with electrodiagnostic medicine. This medical subspecialty uses techniques of a nerve conduction studies with electro myelography (NCS/EMG). Clinical evaluation may reveal some evidence of loss of function, and can include assessment of light touch, the ability to distinguish sharp from dull, the ability to discern temperature, and assessment of vibration. Once a thorough clinical examination is performed, the electrodiagnostic study can be planned. These studies are performed by specially trained neurologist and physiatrists.
If neuropathy is suspected, a search for reversible causes should be done. This can include blood work for vitamin deficiencies or thyroid abnormalities, and imaging studies to exclude a structural lesion impacting the spinal cord. Depending on the results of this testing, there may be a way to decrease the severity of the neuropathy and potentially decrease the pain that a patient is experiencing. Unfortunately, in many conditions, even good control of the underlying cause of the neuropathy cannot reverse the neuropathy. This is commonly seen in patients with diabetic neuropathy.
In rare instances, there may be evidence of changes in the skin and hair growth pattern in an affected area. These alterations may be associated with changes in sweating or perspiration as well. When present, these changes can help identify the probable presence of neuropathic pain associated with a condition called complex regional pain syndrome.
What is the treatment for neuropathic pain?
Various medications have been used in an attempt to treat neuropathic pain. The majority of these medications are used off-label, meaning that the medication was approved by the FDA to treat other conditions and was then identified as being beneficial to treat neuropathic pain. Tricyclic antidepressants (amitriptyline, nortriptyline, desipramine) have been prescribed for control of neuropathic pain for many years. Some patients find that these can be quite effective in giving them relief. Other types of antidepressants have also been shown to provide some relief. Selective serotonin reuptake inhibitors (SSRIs like paroxetine and citalopram) and other antidepressants (venlafaxine, bupropion) have been used in some patients.
Another common treatment of neuropathic pain includes antiseizure medications (carbamazepine, phenytoin, gabapentin, lamotrigine, and others). In severe cases of painful neuropathy which don't respond to first-line agents, medications typically used to treat heart arrhythmias may be of some benefit; however, these can lead to significant side effects and must be monitored closely. Medications applied directly to the skin can provide modest to pronounced benefit for some patients. The forms commonly used include lidocaine (in patch or gel form) or capsaicin. Multiple arguments have been made both promoting and vilifying the use of narcotic agents to treat chronic neuropathic pain. No specific recommendations regarding the use of narcotics will be made at this time.
Curing neuropathic pain is dependent on the underlying cause. If the cause is reversible, then the peripheral nerves may regenerate and the pain will abate; however, this reduction in pain may take many months to years.
What is the prognosis for neuropathic pain?
Many patients with neuropathic pain are able to find some measure of relief, even if their pain persists. Although neuropathic pain is not dangerous to a patient, the presence of chronic pain can negatively impact quality of life. Patients with chronic nerve pain may suffer from sleep deprivation or mood disorders, including depression and anxiety. Because of the underlying neuropathy and lack of sensory feedback, patients are at risk of developing injury or infection or unknowingly causing an escalation of an existing injury.
Is it possible to prevent neuropathic pain?
The best way to prevent neuropathic pain is to avoid development of neuropathy. Monitoring and modifying lifestyle choices, including limiting the use of tobacco and alcohol; maintaining a healthy weight to decrease the risk of diabetes, degenerative joint disease, or stroke; and using good ergonomic form at work or when practicing hobbies to decrease the risk of repetitive stress injury are ways to decrease the risk of developing neuropathy and possible neuropathic pain.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease in which the body attacks the lining tissue of joints, causing chronic joint inflammation. While it primarily affects joints, it can also cause inflammation of organs, such as the lungs, eyes, skin, and heart.
People with RA may experience an increase in symptoms, called "flares," that can last for days or weeks. They may also have periods of remission where they have few or no symptoms. There is no cure for rheumatoid arthritis, but medications can stop the progression of the disease and ease symptoms.
Rheumatoid Arthritis: Are You at Risk?
According to the Arthritis Foundation, rheumatoid arthritis affects about 1.5 million people in the U.S. Women are three times more likely to develop RA than men. Symptoms in women tend to appear between the ages of 30 and 60, while symptoms often develop after age 45 in men.
There may also be a genetic basis for the disease. Cigarette smoking and gum disease (periodontitis) are also risk factors.
- Juvenile Rheumatoid Arthritis (JRA)
- Juvenile rheumatoid arthritis (JRA), also called juvenile idiopathic arthritis (JIA), is a type of arthritis that occurs in children ages 1 to 16.
- Juvenile Rheumatoid Arthritis Symptoms
- Stiff, swollen, painful joints.
- Fever
- Rash
- Juvenile Rheumatoid Arthritis Diagnosis
Healthy Joints vs. Arthritic Joints
Arthritis may refer to more than 100 conditions that affect the musculoskeletal system. Your joints are the places where your bones meet. When arthritis is present, your joints may become inflamed, stiff, red, and painful. Damage from RA may occur in tissues surrounding the joints, including the tendons, ligaments, and muscles. RA is one type of arthritis classified as "systemic," meaning it can occur throughout your body. In some patients, symptoms may extend to the skin and eyes, as well as internal organs, including the lungs, kidneys, heart, and liver.
What Causes Rheumatoid Arthritis?
The exact cause of RA remains unknown, but several risk factors have been identified. Women are diagnosed with RA more often, and it is suspected that the hormone estrogen may play a role. Several studies have shown there is a genetic component to developing RA. Cigarette smoking appears to increase the risk of developing the disease. Occupational exposure to certain dusts such as silica, wood, or asbestos can also lead to a higher risk for developing the illness. Some think there is a viral or bacterial cause of RA but that is still being studied.
Rheumatoid Arthritis Symptoms: Joint Pain
With RA, hands are almost always affected. However, RA can affect any joint in your body, including wrists, elbows, knees, feet, hips, and even the jaw. Usually, joints are affected symmetrically, meaning the same joints on both sides of the body are affected. Rheumatoid arthritis can be very painful, and chronic inflammation can lead to debilitating loss of cartilage, bone weakness, and joint deformity.
Rheumatoid Arthritis Flares
When a person with RA has symptoms including joint inflammation and pain, this is called a flare. Flares may last from weeks to months. This can alternate with periods of remission, when symptoms are minimal to nonexistent. Periods of remission can last weeks, months, or even years. After a period of remission, if the symptoms return this is called a relapse. It is common for RA patients to have periods of flares, remissions, and relapses, though the course of the illness varies with each patient.
Rheumatoid Arthritis Symptoms
In addition to the hallmark symptoms of swollen, painful, and stiff joints and muscles, patients with RA may also experience other symptoms.
Other Symptoms of Rheumatoid Arthritis:
Fatigue
Low-grade fever
Lack of energy
Loss of appetite
Bumps under the skin (rheumatoid nodules)
Shortness of breath due to inflammation or damage to the lungs
Hoarseness
Eye problems
In addition to these symptoms, muscle and joint stiffness of rheumatoid arthritis is usually worse in the morning and after extended periods of inactivity.
Rheumatoid Arthritis Symptoms: Inflammation of Organs
Rheumatoid arthritis is a systemic disease, meaning it can affect the entire body. In addition to the joints and muscles, RA can cause problems in many other areas of the body:
Eyes and mouth: inflammation of the glands in the eyes and mouth causes dryness, and an autoimmune disease of the tear and saliva glands called Sjogren's syndrome. It can also lead to inflammation of the white part of the eye (scleritis).
Lungs: inflammation of the lung lining (pleuritis) or the lungs themselves can cause shortness of breath and chest pain.
Heart: inflammation of the tissue surrounding the heart (pericarditis) can cause chest pain, which tends to be worse when lying down. RA patients are also at greater risk for heart attacks.
Spleen: inflammation of the spleen (Felty's syndrome) can cause a decrease in white blood cells, which raises the risk of infections.
Skin: firm lumps under the skin (rheumatoid nodules), typically located around affected joints, often on pressure points such as elbows, fingers, and knuckles.
Blood vessels: inflammation of the blood vessels (vasculitis) can limit blood supply to surrounding tissues, causing tissue death (necrosis).
What Is a Rheumatologist?
A rheumatologist is usually an internal medicine specialist or pediatrician, with specialized rheumatology training to identify and treat the more than 100 different types of arthritis in addition to other autoimmune disorders such as lupus, polymyositis, and vasculitis.
Rheumatoid Arthritis in Hands
There is no singular test to diagnose rheumatoid arthritis. First, the doctor will perform a physical and take a history of symptoms. The joints will be examined to determine if there is inflammation and tenderness. The heart, lungs, eyes, mouth, and extremities will be evaluated. And the skin may be examined to look for rheumatoid nodules. The doctor may order blood tests or X-rays to help diagnose the condition.
Many other diseases such as gout, fibromyalgia, and lupus may resemble rheumatoid arthritis, so the doctor will rule out these conditions before making a diagnosis of RA.
Rheumatoid Factor & Blood Tests
Blood tests are usually run to help make a diagnosis of rheumatoid arthritis. These tests check for certain antibodies including anti-cyclic citrullinated peptide antibodies (ACPA), rheumatoid factor (RF), and antinuclear antibodies (ANA), which are present in most RA patients.
Rheumatoid factor (RF; a group of antibodies that attack the person’s tissue;) is present in about 75% to 80% of RA patients, and a high RF may indicate a more aggressive form of the disease. Antinuclear antibodies (ANA) is not specific for a diagnosis for RA, but their presence can indicate to the doctor that an autoimmune disorder may be present.
Sedimentation Rate (Sed Rate)
Other blood tests that may be run can help the doctor determine the extent of the inflammation in the joints and elsewhere in the body. The erythrocyte sedimentation rate (ESR, or "sed rate") measures how quickly red blood cells fall to the bottom of a test tube. Typically, the higher the sed rate, the more inflammation there is in the body.
Another blood test that measures inflammation is the C-reactive protein (CRP) test. If the CRP is high, inflammation levels are usually high as well, such as during a flare of rheumatoid arthritis.
Imaging Tests
Another test used to diagnose rheumatoid arthritis is X-ray. Early in the disease, X-rays can be helpful as a baseline test and they can be useful in later stages to monitor how the disease progresses over time. Other imaging tests used include ultrasound and magnetic resonance imaging (MRI).
Arthrocentesis
A joint aspiration procedure (arthrocentesis) may be performed to obtain joint fluid to test in the laboratory. A sterile needle and syringe are used to drain fluid from the joint, which is then analyzed to detect causes of joint swelling. Removing this joint fluid can also help relieve joint pain. Sometimes, cortisone may be injected into the joint during the aspiration procedure for more immediate relief of inflammation and pain.
Osteoarthritis vs. Rheumatoid Arthritis
Currently, there is no cure for rheumatoid arthritis, but there are several medications that can ease its symptoms. Most treatments are aimed at remission, where the patient has few or no symptoms of RA. When treatment is started early in the disease process, this can help minimize or slow damage to the joints and improve quality of life for patients. Treatment usually involves a combination of medication, exercise, rest, and protecting the joints. Sometimes, surgery may be needed.
Medications
If you are diagnosed with rheumatoid arthritis, the sooner the treatment begins, the better your outcome is likely to be. There are many different medications used to help alleviate symptoms of RA and with the goal of bringing a patient into remission.
Common Drugs for Rheumatoid Arthritis
Disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, hydroxycholoquine (Plaquenil), sulfasalazine (Azulfidine, Azulfidine EN-Tabs), leflunomide (Arava), and azathioprine (Imuran)
Biologic response modifiers (another type of DMARD) such as abatacept (Orencia), adalimumab (Humira), anakinra (Kineret), certolizumab and pegol (Cimzia) etanercept (Enbrel), infliximab (Remicade), golimumab (Simponi), and rituximab (Rituxan)
Nonsteroidal anti-inflammatories (NSAIDs) such as ibuprofen (Advil, Motrin), ketoprofen (Actron, Orudis KT), naproxen sodium (Aleve), and celecoxib (Celebrex)
Janus kinase (JAK) Inhibitor – a new drug called tofacitinib (Xeljanz)
Corticosteroids
Analgesics (painkillers)
Drugs used to reduce pain (analgesics) and inflammation (NSAIDs) are often considered "first-line" drugs as they are fast-acting and can relieve symptoms quickly. Medications such as DMARDs and biologic drugs take longer to have an effect, but they can help prevent inflammation and joint damage.
Diet and Rheumatoid Arthritis
While there is no special diet people with rheumatoid arthritis should follow, eating a healthy, balanced diet is always recommended, and some foods may help ease inflammation.
Omega-3 fatty acids found in fish oil may offer anti-inflammatory benefits, so fish such as herring, mackerel, trout, salmon, and tuna may be a part of a healthy diet. If you choose to take fish oil supplements, check with your doctor for the proper dosage.
Extra fiber from fruits, vegetables, and whole grains can result in a lower C-reactive protein (CRP) in the blood. High levels of CRP indicate inflammation.
Vitamin D may help lower the risk for RA in women. Eggs, fortified breads and cereals, and low-fat milk contain Vitamin D.
Rheumatoid Arthritis Treatment for Other Parts of the Body
Rheumatoid arthritis can also affect other areas of the body, and these symptoms may be treated individually.
Sjogren's syndrome can cause eye dryness and may be treated with eye drops to moisturize, and also drops to increase tear production such as cyclosporine (Restasis). Dry mouth related to Sjögren's may be treated with certain mouthwashes and toothpastes.
Inflammation of the lung lining (pleuritis) or the lungs themselves may require treatment with corticosteroids.
Inflammation of the tissue surrounding the heart (pericarditis) usually requires keeping the overall inflammation levels down and many RA drugs can help.
Inflammation of the spleen (Felty's syndrome) can cause a decrease in white blood cells, which raises the risk of infections and may be treated with a stimulating factor (granulocyte stimulating factor/GSF) used to increase the amount of white blood cells.
Rheumatoid nodules may require injections of steroids, or surgery to remove them if they are severe.
Inflammation of the blood vessels (vasculitis) may be treated with painkillers, antibiotics, and protecting the areas affected.
Rheumatoid Arthritis Treatment: Physical Activity and Rest
A balance of physical activity and rest periods are important in managing rheumatoid arthritis. Exercise more when your symptoms are minimal, rest more when your symptoms are worse.
Exercise and Rheumatoid Arthritis
Exercise helps maintain joint flexibility and motion. There are therapeutic exercises with physical therapy that is prescribed, that can help with strength, flexibility, and range of motion of specific joints or body parts affected by your RA. Many recreational activities such as walking swimming are helpful because allow movement with little to no impact on the joints. Consult your rheumatologist or physical therapist to find out what exercises are right for you.
Types of Exercises for Rheumatoid Arthritis
Physicians often recommend the following sports and exercises for their relatively low-stress impact on joints.
- Walking
- Bicycling
- Swimming
- Movement (yoga, tai chi, etc.)
- Strength building
Just as physical activity is important, so is rest. When you have an RA flare and your symptoms are worse, it is best to reduce your activity to help minimize joint inflammation and pain, and to cope with fatigue.
Surgery for Rheumatoid Arthritis
With severe rheumatoid arthritis, surgery may be needed to reduce pain and improve joint function. Some surgeries include joint replacement, fusion of joints (arthrodesis), tendon reconstruction, and removal of inflamed tissues (synovectomy). Discuss your treatment options with your doctor at Bothwell Medical Rooms to find out what is right for you.